Definition of "Fluid replacement"
Fluid replacement is the replenishment of bodily fluids lost through various means (sweating, bleeding, fluid shift, or other pathological processes).
Patient information
What is fluid replacement?It's where we replenish the body with fluids. This happens constantly, as we lose water through sweat, bleeding, fluid shift, or some other sort of diseased thing. We do this naturally, by... just drinking water
 .
.It includes:
- Oral rehydration therapy (drinking). Examples of oral rehydration solution to Tx dehydration, including Hydralyte, Gastrolyte

Source: 2013/07/Hydralyte.jpg">Pharmacy Daily

Source: 2014/01/05/fmimg5239194285916251315.jpeg">CBSI
- Intravenous therapy (aka drip), which is the fastest way to deliver fluids and medications throughout the body. it employs a drip chamber, which prevents air from entering the blood stream forming an air embolus, and allows an estimation of flow rate
- Rectally (e.g. with a Murphy drip)
- Hypodermoclysis (aka interstitial infusion, subcutaneous infusion, i.e. direct injection of fluid into subcutaneous tissue)
Patient information
So you mentioned we can replenish fluid by drinking water. What else can we do?So we can do it with water, or we can do it with hydralyte or gastrolyte, which are specially formulated fluids with electrolytes. You can also do it through blood, called IV or drip. Up the buttock. Or under skin.
Note that the fluid indications are independent of another, meaning they are a combination of, rather than "either":
- Resuscitation fluids, where the Pt is hypovolemic due to dehydration, blood loss, or sepsis, and requires urgent IV to correct the deficit. It is provided as a bolus. Fluid challenge is where a small amount of fluid (250mL) is given initially to see the Pt's response. It is reserved for hemodynamically unstable Pt's
- Constituency: 0.9% NaCl, with NO glucose or KCl → rapid K administration is harmful to the heart. Same for neonates
- Rate: Healthy adults: 500mL bolus. Elderly/cardiac problems: 250mL bolus. 20mL/kg bolus. In neonates, 10-20mL/kg bolus
- Rehydration/Replacement fluids, where lost fluid is replaced. It should not be provided in anticipation
- Constituency: Same as maintenance, namely 0.9% NaCl + 5% glucose +/- 20mmol/L KCl. In neonates, same as maintenance, namely, 0.45% NaCl + 10% glucose +/- 10mmol/500mL bag KCl
- Rate: (Weight in kg * % clinical dehydration * 10mL) per day, where % clinical dehydration depends on a table, ranging from 0 for "No clinical signs of dehydration" (reduced urine output, thirsty), 3% for "Mild" (+dry mucous membranes, mild tachycardia), 5% for "Moderate" (+tachycardia, abnormal respiratory pattern, lethargy, reduced skin turgor, sunken eyes), 10% for "Severe" (+signs of poor perfusion including or shock)
- Maintenance fluids (Maint), where the Pt is at negligible loss
- Constituency: 0.9% NaCl + 5% glucose +/- 20mmol/L KCl. In neonates, we give half the salts and double the glucose, namely, 0.45% NaCl + 10% glucose +/- 10mmol/500mL bag KCl
- Rate: In adults, approximately 100mLs/hr, which is 2.4L/day. Total maintenance per hour in kids is calculated either by 2 rules, which are NOT equal:
- 4, 2, 1 "hourly" rule, i.e. 4mL/kg/hr for the first 10kg, +2mL/kg/hr for the next 10kg, +1mL/kg/hr for every 1kg of the Pt's weight thereafter, up to a maximum of 2.5L/day
- 100, 50, 20 "daily" rule, i.e. 100mL/kg for the first 10kg + 50mL/kg for the next 10kg + 20mL/kg for every 1kg of the Pt's weight thereafter, up to a maximum of 2.5L/day
- The 100, 50, 20 rule may be easier to remember because the "2" and "5" and "00" can be obtained from the prior numbers, which equates 2500mL=2.5L
Source: 2009-8070.pdf">NSW Health
Patient information
So there are 3 sorts of fluids? Resus, replacement, and maintenance?Resus is given when there's been a big loss of blood, which happens in dehydration, blood loss, and blood infection. Replacement is given when there's been a loss, but not to that same degree, such that we're only a bit dehydrated here. Maintenance fluid is where there has been no loss, but you're just "topping up" because the patient is not or cannot drink water, so you give it by IV.
What's in them? Do you give the same thing for everyone? Is it just water?
When we give a big lot, we give salty water. We don't add anything to it, like glucose. In fact, given potassium super fast is dangerous to the heart. For both replacement and maintenance, we usually add glucose, and we can also add potassium too.
That's like giving everyone, except those who you give a bolus, a banana. Bananas are high in sugar and potassium  . Is it different little babies?
. Is it different little babies?
Same stuff, just half the salt, double the sugar.
That's sound like the sort of things kids would like  . How fast do you give these fluids?
. How fast do you give these fluids?
So resus is all at once, because they really need it. Replacement depends on dehydration and weight. Maintenance is based on the 4-2-1 or 100-50-20 rule.
Wait... why is there no "rate" listed for resus fluids?
That's what the word "bolus" is there for. It means it's give as fast as possible. So you could think of the rate being 99999mL/hour  We give it so quickly we usually write it as "stat", which means it's all been given right now
We give it so quickly we usually write it as "stat", which means it's all been given right now  ! But we don't give the same amount of sudden fluids to everyone. We give 2 cups, or 500mL in adults. But for those who are old or have haert problems, we give 1 cup only, 250mL.
! But we don't give the same amount of sudden fluids to everyone. We give 2 cups, or 500mL in adults. But for those who are old or have haert problems, we give 1 cup only, 250mL.
- Crystalloids, are solutions containing small molecules that can easily cross cell membranes. It includes:
- Normal saline (NS) 0.9% w/v NaCl, which contains 154mmol/L of Na and Cl per 1L. Bags containing KCl are also available, usually either 20mmol/L or 40mmol/L
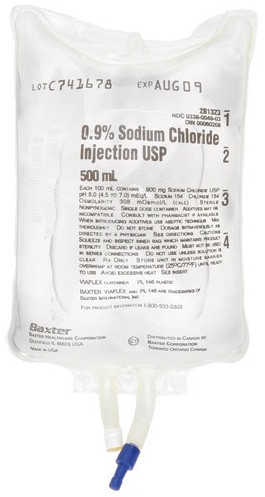
Source: Lucky Pharmacy Liberia
Patient information
What's in Normal Saline? Is it just salty water?Yeaaap! It's exactly as it sounds. It is 0.9% w/v NaCl, which if you use the periodic table numbers, will get you, in a 1L bag, 154mmol of Na+ and 154mmol of Cl-.
-
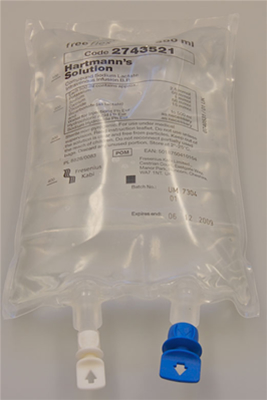
- Hartmann's [solution] (aka compound sodium lactate, CSL), which contains 131mmol/L Na, 111mmol/L Cl, 29mmol/L HCO3 (in form of lactate), 5mmol/L K+, 2mmol/L Ca2+ per 1L. It is more closely isotonic w/ blood than normal saline. It is used to replace body fluid and mineral salts that may be lost. It is especially suitable when losses cause acidemia. It is relatively contraindicated in Pt's with DM, as one of the isomers of lactate is gluconeogenic
- 5% Glucose or dextrose, which is a solution w/ sugar, where it may function both as a means of maintaining tissue hydration, and a means of parental nutrition. Types include:
- D5W (5% dextrose in water), which consists of 278mmol/L dextrose
- D5NS (5% dextrose in normal saline), which in addition contains NS (0.9% w/v of NaCl). Alternatively, D51/2NS, contains 5% dextrose (50g/L) in 1/2 the amount of NS (0.45% w/v of NaCl, or 154/2=77mmol/L Na and Cl)
Source: e-Safe anesthesia
Patient information
Alright, what's Hartmann's then? And how's it different from Normal Saline?It's more similar to blood (which in turn is similar to ECF), even with the Na and Cl. It has 131mmol Na+, 111mmol Cl-. In addition, it has 29mmol HCO3- (bicarbonate), 5mmol K+, and 2mmol Ca2+. So in addition to the salt, it has bicarbonate, potassium, and calcium. But it's still all within a 1L bag of water.
Source: 2015/10/electrolytescompositionextracellularintracellularcompartments-f10_01.gif">Toddlee MD
ECF is extracellular fluid. What is that, and how's that different from intracellular fluid?
ECF is fluid outside cells. ECF includes blood plasma, along with interstitial fluid. Intracellular fluid is fluid inside cells, which is mostly cytosol, where organelles are suspended.
5% glucose? That's sugary rather than salty water?
No. It's sugar in salt water. 5% glucose has 50g of glucose. Carbs have 4 calories per gram, so 50g glucose has around 200 calories. If it's prepared from dextrose, it only has 3.4 calories per gram, so 50g dextrose would have 170 calories.
- Colloids, which contain larger molecules, such as gelatin or albumin, that remain within the intravascular space. They are thought to expand the intravascular space for a longer duration than the crystalloids. They are becoming less used because of their risk of anaphylaxis, and because in practice crystalloids are actually just as effective
- Blood products, which are ordered from the transfusion lab. It includes:
- Packed red cells
- Platelets
- Fresh frozen plasma (FFP)
- Pain
- Infection
- Phlebitis
- Infiltration/extravasation
- Fluid overload, which occurs when fluids are given at a higher rate, or in a larger volume, than the system can absorb or excrete. This can cause:
- HTN
- Heart failure
- Pulmonary edema
- Hypothermia
- Electrolyte imbalance
- Embolism
- Glucose, for energy
- Measure hourly urine output and input
- Closely monitor U&E, and adjust fluid type accordingly
- Fluid requirement is higher in younger kids, per kg, as indicated by the 4-2-1 rule, because of immature renal function
The paperwork for Pediatric daily fluid balance chart includes:
- Affix Pt label
- Date: __/__/____
- Instructions for Use include All entries must be legible and written in black pen. IV Site/s Check - refer to local policy in relation to IV site check requirements. Urine and Vomitus Outputs - if it is usual business practice to record progressive totals please draw a diagonal line in the field and write the progressive total below the diagonal line. IV line change due ___. PT = Progressive Total
- Date: __/__/___
- Instructions
- Daily weight
- There is a large table, which on the very LHS includes the Time, ranging from 0100, 0200, 0300... 2200, 2300, 2400, followed by Subtotal for that column. The various columns for the according times are:
- Under Input set of columns, Line A site (Solution and Volume have different cells), Line B site (Solution and Volume have different cells), Line C site (Solution and Volume have different cells); Parenteral total (P); IV Site/s Check, IV Press mmHg, Oral/Enteral (OE) (with cells for Type, Route, Fluid Volume), Expressed Breast Milk (EBMI) signature (which requires countersign); Oral/Enteral total (OE); Progressive total in (P+OE=X)
- Under Output set of columns, Urine/PT, Vomitus/PT, Gastric Aspirate, Drain 1 (with an additional cell underneath); Fecal/Other; Progressive total out (Y); Progressive Fluid Balance (X-Y)
- At the bottom row, Total input (X), Total output (Y), Total balance (X-Y)
- All entries must be legible and written in black pen. Also a note for, Note: Consider insensible losses
The paperwork for Pediatric IV fluid order chart includes:
- Includes note that Rechart fluids orders at least daily, and Calculate all fluids on current weight
- Affix Pt label
- First prescriber to print Pt name and check label correct: ____
- Weight (kg)
- Date weighed
- Height (cm)
- B.S.A. (m^2) (body surface area)
- Gestational age at birth (wks)
- Calculation of IV fluids, NB: Refer to Page 2 for assistance; MO to complete. Under:
- (A) Maintenance, if >28 days, 1st 10kg = ___mL, 11-20kg=___mL, >20kg=___mL, Total=___mL. If <28 days, For neonates <=2 weeks of age use birth weight if admission weight is less than birth weight. Total maintenance/24hr= ___mL
- (B) Replacement, if >28 days, (Only replace volume to a total of 5% in 1st 24 hrs), =___mL, Ongoing losses = ___mL. Total = ____mL. Or if <28 days, =___mL
- (C) Total proposed fluids, (A+B)=___mL/24 hrs = ___mL/hr
- Allergies/Adverse drug reactions (ADR)
- Table, which includes the columns Date/Time __/__/____, Route/Line, Fluid type, Additive and dose, Total volume, Rate (mL/hr), Prescriber's Name Print & Signature / pager No. (3 boxes available in total), Date/Time Started __/__/____, Date/Time finished __/__/____, Administered print/sign (2 boxes), Checked print/sign (2 boxes)
- Note that, Use this form in conjunction with relevant local pediatric clinical guidelines
- Notes on the back, including:
- 1. Resuscitation fluids (not to be included in the 24 hour maintenance fluid total). Neonates - 10-20mL/kg bolus 0.9% sodium chloride (no glucose) then reassess. Infants and Children - 20mL/kg bolus 0.9% sodium chloride (no glucose) then reassess. Hartmann's solution OR Plasma-Lyte 148 (NO glucose) (specialist directed) then reassess
- 2. Maintenance fluid, which includes the columns Pt age/weight, Daily IV requirements, Hourly IV requirements, Fluid type
- Under Neonatal, for Day 1 of life, daily 60mL/kg, hourly 2.5mL/kg, and type 10% glucose/500mL. For Day 2 of life, daily 90mL/kg, hourly 3.75mL/kg, and type 0.225% sodiu mchloride + 10% glucose/500mL OR 0.45% sodium chloride + 10% glucose/500mL, WHERE there is pre-existing hyponatremia (sodium less than reference range), or increased risk of hyponatremia - such as sodium loses (e.g. gut) or high risk of non-osmotic ADH secretion (e.g. post-op, respiratory illnesses, CNS disease)
- Under >28 days, for 3-10kg, daily 100mL/kg, hourly 4mL/kg. For 10-20kg, daily 100mL+ (50mL/kg for each kg over 10kg), hourly 40mL+(2mL/kg/hr for each kg over 10kg). For >20kg, daily 1500mL+(20mL/kg for each kg over 20kg), hourly 60mL+(1mL/kg/hr for each kg over 20kg). All of the following had type 0.45% sodium chloride + 5% glucose with or without potassium chloride 10mmol/500mL OR 20mmol/1000mL; OR 0.9% sodium chloride + 5% glucose with or without potassium chloride 10mmol/500mL OR 20mmol/1000mL WHERE there is pre-existing hyponatremia (sodium less than reference range), or increased risk of hyponatremia - such as sodium losses (e.g. gut) or high risk of non-osmotic ADH secretion (e.g. post-op, respiratory illnesses, CNS disease); OR Plasma-Lyte148 + 5% glucose (Children's Hospital ONLY)
- 3. Replacement fluid, where Calculation of deficit: Volume in mL=weight (kg) * % dehydration * 10. replace deficit at a constant rate over 24 hrs. Only calculate replacement volume to 5% dehydration in the first 24 hours. Fluid type:
- Neonates: 0.45% sodium chloride + 10% glucose with or without potassium chloride 10 mmol/500 mL OR 0.9% sodium chloride + 10% glucose with or without potassium chloride 10 mmol/500mL
- Infants and children: Infants and children: 0.9% sodium chloride + 5% glucose with or without potassium chloride 10 mmol/500mL OR 0.9% sodium chloride 5% glucose with or without potassium chloride 20 mmol/1000mL OR Plasma-Lyte148 + 5% glucose (Children's Hospitals ONLY)
- Ongoing GI losses: Measure and replace over an hourly or 4 hourly period
- Sample calculation of fluid deficit (for 24 hrs). Child with gastroenteritis: weight =22kg, estimated dehydration=5%. The majortiy of children will not require rehydration of more than 5% deficit in the first 24 hrs. Maintenance Fluid: For 22kg: 1500mL + (20mL/kg * 2) = 1540mL (A). Replacement deficit: 22kg * 5% * 10 = 1100mL (B). Total fluid replacement: 1540+1100=2640mL/24hr (C). =110mL/hr
- Consultation with a senior clinicial required for infants and children with, greater than or equal to 10% dehydration; infants less than 3 months of age (corrected for gestation) or <5kg; glucose, sodium or potassium outside of noral range; a need for rapid IV rehydration (e.g. over 4 hours) as per Gastroenteritis Clinical Practice Guideline; conditions where fluid balance is complex and critical: diabetic ketoacidosis (DKA), meningitis, cardiac failure, head injury, sepsis, severe burns, acute abdominal pain, renal insufficiency or kidney disease hypernatremic dehydration, metabolic disorers, syndrome of inappropriate antidiuretic hormone (SIADH); ongoing fluid losses; any other concerns about fluid requirements
- Monitoring guidelines: Fluid requirements must be reassessed AT LEAST every 24 hrs, after review of clinical/electrolyte status; if child's condition deteriorating (or not improving) consider more frequent reviews. Check serum electrolytes at the start of therapy and at least 24 hourly if maintenance IV therapy continues; if child not improving consider checking electrolytes more frequently. Blood Glucose Level (BGL) should be monitored as needed. Ensure accurate fluid balance chart. Weight on admission and then daily if receiving maintenance IV fluids
Paperwork for Parent administration of oral fluid (pediatric) includes:
- Affix Pt label
- Oral fluids for your child with gastroenteritis, includes (1) small and frequent breast feeds OR (2) oral rehydration therapy e.g. gastrolyte or hydralyte (fluid or ice block) OR (3) dilute juice (if ORS is refused) - 1 part apple juice to 4 parts water
- Your child's weight is: ___kg
- Your child should drink ___mLs every 5 minutes (0.5mL/kg). NB: For breastfeeding babies please write length time spent breastfeeding (i.e. number of minutes)
- Use the measuring cup or syringe to measure the fluid (One Hydralyte iceblock = 62.5mL)
- Give the fluid to your child to drink with a syringe, teaspoon, cup or bottle
- Parent administration of oral fluids not to exceed 2 hours without seeing a doctor
- Table, with the columns:
- Date (every 5 minutes write down how much your child drinks, and if they toilet), and Time
- For In, Type of fluid your child drinks (e.g. breast milk, juice, hdyralyte), and Amount your child drinks (mLs or minutes breastfeeding)
- For Out, Tick if your child vomits, Tick if your child passes urine (toilet or wet nappy), Tick if your child has diarrhea
- Totals at the very bottom row, for In, and Out
- On the other side, Oral fluids for your child with gastroenteritis, information. The nurse who assessed yoru sick child has placed your child into an appropriate category for urgency to see the Dr. Based on the Hx you gave, it is presumed that your child has gastroenteritis and will require fluid Tx. Here at the ED, we use the waiting period before a Dr is able to see your child to trial oral fluids. Giving small amounts of correctly diluted fluid regularly is often successful in corrected dehydration in children. The other side of this sheet explains exactly how much fluid and how often we wnt you to give it to your child. When your child sees a Dr a decision will be made as to whether you can go home, or whether your child needs a small tube through the nose into the stomach or a drip to provide extra fluid for a few hours. This will happen here in the ED. Sometimes this is all it takes to make your child feel a lot better and you will then be able to go home. If this fails to improve your child, he or she may need to be admitted to hospital for further Tx
- The Dr will assess and decide whether or not your child needs admission to hospital. This assessment may include The need to have some blood and urine tests, The need to be given fluids through a naso-gastric tube or drip. A NG tube is one that passes from the nose to the stomach through whic fluids are given. This is a safe and effective way of giving fluids and is often less distressing compared with a drip. If this is not suitable or unsuccessful your child may need a drip. If your child is able to go home, Continue to give small amounts of fluid frequently, Continue to breastfeed but make sure you offer addiitonal fluids 1-2 hourly
- Approximate volumes of fluid to give, include from 6-23 months, 40-60mL each hour. 2-5yo, 60-100mL each other. 6-10yo, 100-120mL each other. 11-16yo, 120-160mL each hour
- Saline solution
- Hartmann's procedure (do NOT confuse)
Find a practitioner
Practitioner count: 0